Have you ever been on a low-fat, or calorie-restricted diet to achieve weight loss?
Do you feel severely bloated or uncomfortable after eating difficult to digest meals, such as those containing high levels of fats?
Most people, especially women, will answer yes to the first – however, if you answered ‘yes’ to both, I’m going to tell you how these two questions could be related, and how a low-calorie, low-fat diet may be damaging your digestion more than helping it.
My Confusing Experience with Fat Consumption and Bloating
At the start of my own personal 24/7 bloating experience, I was determined to remain on a low-fat diet consisting of easily digestible foods, as is often promoted for people with digestive disturbances. I stuck to it strictly – yet, my bloating only seemed to get worse by the month. I’d wake up after a meal of rice-pasta and tomato sauce looking like I had ate two Christmas dinners with a baby on the way.
I was terrified of eating fats because when I would, the bloating would get even worse and I was actually able to see the poor digestion, indicated by floating stools (apologies for getting graphic, but those who are reading the post due to chronic bloating will, I’m sure, prefer to know all of the signs to accurately solve their issue).
The even more confusing thing is that, on the rare occasion that I ate plenty of fats in one meal – things would calm down the next day. Why was this so confusing? Why were small amounts of fat seeming to make things worse than if I ate a non-fat diet, yet when I over-consumed fat in one sitting, my bloating would calm down?
Was I hitting some sort of biological bloating threshold? What the heck was going on?
It turns out, my years of typical low-fat, low-calorie dieting may have been a major culprit in contributing to my chronic bloating issues.
To understand why, you first have to understand the role of the gallbladder in fat digestion.
The Gallbladder: An Essential Digestive Organ
The gallbladder is one of your organs responsible for secreting digestive fluids, namely bile, in response to detecting food in the stomach.
The gallbladder is immensely important, as it secretes fluids that provide some of our greatest aid for breaking down difficult to digest meals, such as those containing high levels of fat.
When fat is present in the stomach, the gallbladder contracts and ejects a large proportion of bile to assist digestion, however when little or no fat is present, the gallbladder releases minimal amounts of bile1,2,3,4,5, as the aid of such digestive fluid is not highly necessary.

This detection process works great when your diet is varied and balanced – however, several issues can arise when you’re on a consistently low-fat diet for an extended period of time.
Low-fat Diets may Cause Digestive Danger
After shuffling through research, I easily found piles of studies that contradict – even warn against – popular ‘low-fat’ dietary trends.
I realize some of the information I’m about to give you may seem counter-intuitive, but please know that this is critically analyzed scientific evidence (not opinion), and this information is actually common knowledge amongst the world of highly qualified nutritional scientists such as myself. Think about it – if we didn’t know more than the general public, then everyone would have perfect digestion and their dream body, right?
It is apparent in literature that low-fat meals do not result in maximal emptying of the gallbladder1,2,3,4,5. This makes sense because, as you just learned, the gallbladder is sensitive to fat content and secretes appropriate amounts of digestive fluids to digest a given meal.
Additionally, low-fat meals produce reduced stimulation of CCK, a hormone which stimulates the release of bile into the intestine and the secretion of pancreatic enzymes6.
When it comes to making low-fat dieting a lifestyle, several studies have demonstrated that long-term, low-fat, low-calorie diets resulting in poor gallbladder emptying actually promote stagnant bile1,2,3,4. The layman’s term for this is “sticky bile”, and the consequence is that bile isn’t able to eject as easily from your gallbladder when it actually needs to, thus impeding normal digestion.
Through these gallbladder influences, low-fat, low-calorie diets can over time contribute to poor digestion, significant bloating, and have even shown to drastically increase the probability of gallstone formation, especially in obese individuals whose bile becomes saturated with cholesterol3,4,7.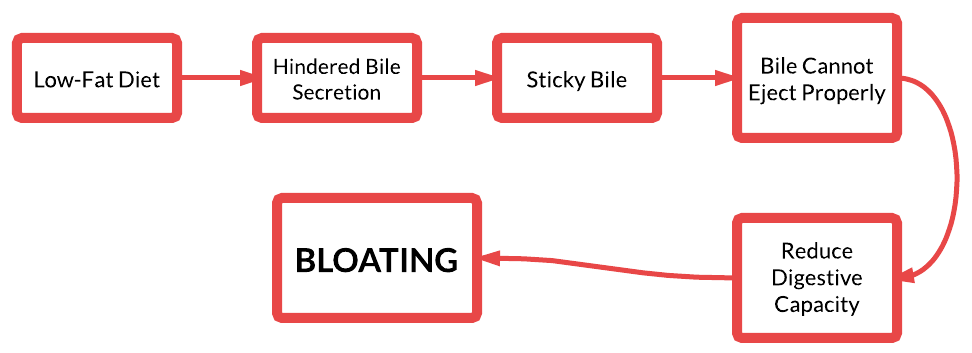
The Digestive Balancing Act
When embarking upon a journey to return your gallbladder to a working status, there’s a very particular balance you must achieve: the balance between consuming enough fat to encourage gallbladder emptying, while consuming little enough that your body can process the fat without aggravating your current digestive status.
Since your gallbladder simply won’t be up to the task of easily ejecting bile or digesting large amounts of fats, the use of supplementary nutritional help will be the key for revving up your gallbladder functionality while minimizing any symptoms of bloating and digestive distress.
So today, I’m going to fill you in on how to safely and effectively kick-start your gallbladder to encourage digestive repair and kick bloating to the curb for good.
3 Steps to Kick-starting Your Gallbladder for Optimal Digestion
1. Consume a minimum of 10g fat per meal
Several studies have shown that consuming a minimum of 10g fat per meal results in maximum gallbladder emptying4,8. This may be much more than some digestion sufferers or dieters are used to (non-fat every-thang), however if you’re eating 3 meals a day, this only adds up to 30g fat, which is still considered quite low. Studies have shown higher proportions of fats to achieve potentially greater effects such as significantly greater CCK stimulation and gallbladder contraction6, however if you’re experiencing bloating and digestive distress in response to fats, it may be a good idea to begin with the minimum quantity of 10g and work your way up. If you’re worried about weight gain from increasing fat – don’t be! Check out this article to understand how to properly increase fat in a way that actually promotes weight loss. To give you an idea, in some of my least-bloated and slimmest days, I was consuming well over 100g fat daily – although this quantity is not right for everyone, and definitely excessive for those experiencing bloating as part of certain severe digestive disorders.
2. Supplement with Lipase
Lipase is a digestive enzyme necessary for processing fats or “lipids”. Supplementing with lipase is an effective strategy for those experiencing fat digestion issues, which can be indicated by floating stools or worsening of bloating and digestive symptoms following fat consumption9,10,11,12,13. This doesn’t mean just using a digestive enzyme that includes lipase (most typically do), but actually supplementing with a highly concentrated lipase formulation in addition to your digestive enzymes. I’ve tried several brands, but this brand* was one of the biggest breakthroughs I had, as after nearly a year of chronic bloating with little relief, it dramatically calmed things down overnight. In fact, the following doctor I saw was so impressed with the quality and improvements this supplement made, that he started ordering it and using it regularly with his own patients. I started off by taking 3 lipase capsules with each meal, in addition to my regular dose of digestive enzymes.
*If Amazon doesn’t deliver to your area, email me and I will get it shipped to you direct from a dispensary. It helped me a lot, and I want to make sure you have access to the same help wherever you’re located.
3. Beetroot
Beetroot provides one of the richest food sources of betaine, which stimulates the release of bile by attenuating any blockages or reductions in bile flow14,15. Beets can be consumed whole, however to increase potency and efficacy, delivery through the use of beetroot juice or concentrated daily supplementation can significantly enhance therapeutic effects. The best brand I’ve used was by Empirical Labs called Beet Flow, which I took 2 capsules of with each meal. It’s not the cheapest, and I haven’t found it on any trusted websites I could share such as Amazon as this product is typically supplied directly from a practitioner – however, you can Google the product and will find various supplement websites that distribute it. If you want to go the juicing route, you can either juice fresh beets, or use an all-natural concentrated beetroot powder to enhance portability and convenience (and avoid staining a million outfits like I did).

The Key Ingredient: Patience
Overall, these interventions provide a well-rounded protocol for kick-starting your fat digestion after long stints of low-fat dieting that may be behind your bloating. Increasing the fat content of each meal will stimulate your gallbladder to contract and eject more digestive fluids, while the use of beetroot will assist in the thinning and stimulation of bile flow in order to promote the movement of stagnant bile and encourage maximal gallbladder emptying. Additionally, as your digestion may currently be sensitive or weak, supplementation of lipase will allow you to process the fat contained in each meal, in order to attenuate bloating and digestive distress that may accompany fat-containing meals.Remember, increase your fat content gradually and expect some discomfort along the way. Your digestion is likely weak, and it will take time to undo years of low-fat dieting and other accumulated damage. To give you an idea, although I began experiencing the symptomatic benefits of this protocol almost immediately, the actual reparation of my fat digestion took several months until I was able to stop supplementing with lipase completely. I’m happy to report that my fat digestion is now working at full capacity, but I still consume beets regularly because wow are they delicious!
Be persistent with your health, but be patient also. The gut is a timely organ to repair – but it will be worth it in the long-run.
Health begins in the gut,
Anita Tee
MSc Personalized Nutrition; BSc Genetic & Molecular Biology
Personal Training Specialist; Canadian Register of Exercise and Fitness Professionals
References:
1. Perreard M, Iconomidis N, Bernard C, Chayvialle J, Gerolami A. Effect of a low-fat diet on the fasting volume and postprandial emptying of the gallbladder. Gastroenterol Clin Biol. 1993;17(6-7):435-40.
2. Marzio L, Capone F, Neri M, Mezzetti A, De Angelis C, Cuccurullo F. Gallbladder kinetics in obese patients. Effect of a regular meal and low-calorie meal. Dig Dis Sci. 1988;33(1):4-9.
3. Festi D, Colecchia A, Orsini M, Sangermano A, Sottili S, Simoni P et al. Gallbladder motility and gallstone formation in obese patients following very low calorie diets. Use it (fat) to lose it (well). Int J Obes Relat Metab Disord. 1998;22(6):592-600.
4. Gebhard R, Prigge W, Ansel H, Schlasner L, Ketover S, Sande D et al. The role of gallbladder emptying in gallstone formation during diet-induced rapid weight loss. Hepatology. 1996;24(3):544-548.
5. Stone B, Ansel H, Peterson F, Gebhard R. Gallbladder emptying stimuli in obese and normal-weight subjects. Hepatology. 1992;15(5):795-8.
6. Froehlich F, Gonvers J, Fried M. Role of nutrient fat and cholecystokinin in regulation of gallbladder emptying in man. Dig Dis Sci. 1995;40(3):529-33.
7. Stokes C, Gluud L, Casper M, Lammert F. Ursodeoxycholic Acid and Diets Higher in Fat Prevent Gallbladder Stones During Weight Loss: A Meta-analysis of Randomized Controlled Trials. Clinical Gastroenterology and Hepatology. 2014;12(7):1090-1100.e2.
8. Vezina W, Grace D, Hutton L, Alfieri M, Colby P, Downey D et al. Similarity in gallstone formation from 900 kcal/day diets containing 16 g vs 30 g of daily fat: evidence that fat restriction is not the main culprit of cholelithiasis during rapid weight reduction. Digestive Disease Science. 1998;43(3):554-61.
9. Hornsby V. Floating faeces in steatorrhoea — A new sign. Clinical Radiology. 1988;39(6):692.
10. Keller JLayer P. Pancreatic enzyme supplementation therapy. Curr Treat Options Gastro. 2003;6(5):369-374.
11. Solomon S, Whitcomb D, LaRusch J. PRSS1-Related Hereditary Pancreatitis. GeneReviews. 2012;.
12. Domínguez–Muñoz J. Chronic Pancreatitis and Persistent Steatorrhea: What Is the Correct Dose of Enzymes?. Clinical Gastroenterology and Hepatology. 2011;9(7):541-546.
13. Whitcomb D, Lehman G, Vasileva G, Malecka-Panas E, Gubergrits N, Shen Y et al. Pancrelipase Delayed-Release Capsules (CREON) for Exocrine Pancreatic Insufficiency due to Chronic Pancreatitis or Pancreatic Surgery: A Double-Blind Randomized Trial. Am J Gastroenterol. 2010;105(10):2276-2286.
14. Graf D, Kurz A, Reinehr R, Fischer R, Kircheis G, Huassinger D. Prevention of bile acid–induced apoptosis by betaine in rat liver. Hepatology. 2002;36(4):829-839.
15. Kim Y, Jung Y, Kim S. Effect of betaine supplementation on changes in hepatic metabolism of sulfur-containing amino acids and experimental cholestasis induced by α-naphthylisothiocyanate. Food and Chemical Toxicology. 2005;43(5):663-670.

Anita Tee
My name is Anita Tee. I'm a nutritional scientist who specializes in histamine intolerance. I hold a Master of Science in Personalized Nutrition and a Bachelor of Science in Human Biology and Psychology.For the past ten years, I have used my experience in nutritional and medical health sciences to create a scientifically backed, natural approach to healthcare that relies 100% on evidence-based research.As I previously suffered from - and overcame - histamine intolerance, my focus is to increase recognition and expand the available resources and protocols available for resolving this particular disorder. To date, I have helped over 4,000 individuals fully resolve or better manage their histamine intolerance symptoms.